Medicare and Medicaid are two different government programs for healthcare. It is important to understand…
Levels of Appeal on a Denied Health Insurance Claim
Navigating the rules and limitations of your health insurance policy can be a daunting task, and understanding the process of appealing a denied claim is no exception. If you receive a claim denial letter from your health insurance company and choose to appeal the decision, you may be wondering how long the process will take and who gets to make the decisions at each stage. For most employer-sponsored health care plans, there are at least two levels of administrative appeal, and sometimes more if your insurer has a multi-level internal appeals process.
NOTE: The following information applies to private, employer-sponsored insurance plans. Government-sponsored plans, such as Medicaid, Medicare, TRICARE, the federal employees’ health benefits program, etc. have their own appeals processes and are subject to different rules. Medicare, for example, has 5 levels of appeal, which are outlined here.
Internal Appeal
At the first level of appeal, known as an internal appeal, you or your healthcare provider will submit a request for reconsideration to your insurance company. This process happens entirely within your insurance company, without the involvement of independent reviewers or government agencies.
In lieu of a formal appeal, your physician may request a “peer-to-peer review,” in which your physician will have a telephone conference with a medical reviewer working for your insurance company to explain why the services you received–or will receive–are medically necessary, and should therefore be covered under your plan. In some cases, this can result in a reversal of the denial, saving you the trouble of filing a formal appeal.
You can expect a decision on an internal appeal within 30 days for a prior authorization; or up to 60 days for services already received. In urgent cases, you may request an expedited appeal, which your insurer must decide upon within 72 hours.
Depending on your plan, there may only be one level of internal appeal, or there may be more. A second-level internal appeal, for example, will typically be made by a medical reviewer working for your carrier who did not participate in the initial claim decision. Under most circumstances, you must go through each level of internal appeal before you can request an independent external review.
Note: In Virginia, exceptions to the external review rule can be made when an insurance company fails to decide upon an appeal within 30 or 60 days (depending upon whether the appeal is for pre-authorization or services already rendered), or if an expedited external review is merited due to a patient’s urgent medical needs. See our Guide to Health Insurance Appeals for more information about expedited appeals. Under such circumstances, one may file for an expedited internal review and expedited external review simultaneously.
External Review
If you have exhausted the internal appeals process and the insurance company still won’t approve your claim, you or your authorized representative may request an independent external review.
Your insurance company’s final denial letter must include instructions on how to request an external review, which varies by state. For plans that use Virginia’s external review process, external review requests must be filed with the Virginia Bureau of Insurance within 120 days of receipt of a final adverse determination (a.k.a. denial of your internal appeal).
Once you have submitted a request for an external review to the Bureau, it will notify your health carrier. Your carrier may, in turn, request more information from you to verify your claim is eligible for an external review. All requested information must be submitted to your carrier within the timeframe they specify, or else your review request may be rejected.
If your completed request is deemed eligible for external review, the Bureau will randomly select a third-party organization, called an Independent Review Organization (IRO), to review your claim. An IRO, by law, must have no apparent financial incentive to decide in favor of either you or your insurance company.
If your request is deemed ineligible, you may appeal the decision with the Bureau. After an IRO is chosen and you are notified of its name, you will have only five business days to submit any further information you would like to be considered in the determination process.
Decisions on standard external appeals are due within 45 days of the Bureau’s receipt of your request, or within 72 hours if the review is expedited. Once an IRO has issued its determination, it is binding upon your carrier—meaning, if the IRO overturns a denial, your insurer is legally obligated to pay for your claim.
Beyond Administrative Appeals
If an IRO upholds your insurer’s initial determination, the only chance you have of getting your insurer to pay for the claim is by bringing the issue to court. If you have reached the end of the administrative appeals process without success and still believe your claim should be covered, Norton Health Law can help. We know firsthand that health insurance companies will do everything possible to avoid paying what is owed, which is why we are prepared to aggressively represent your best interests.
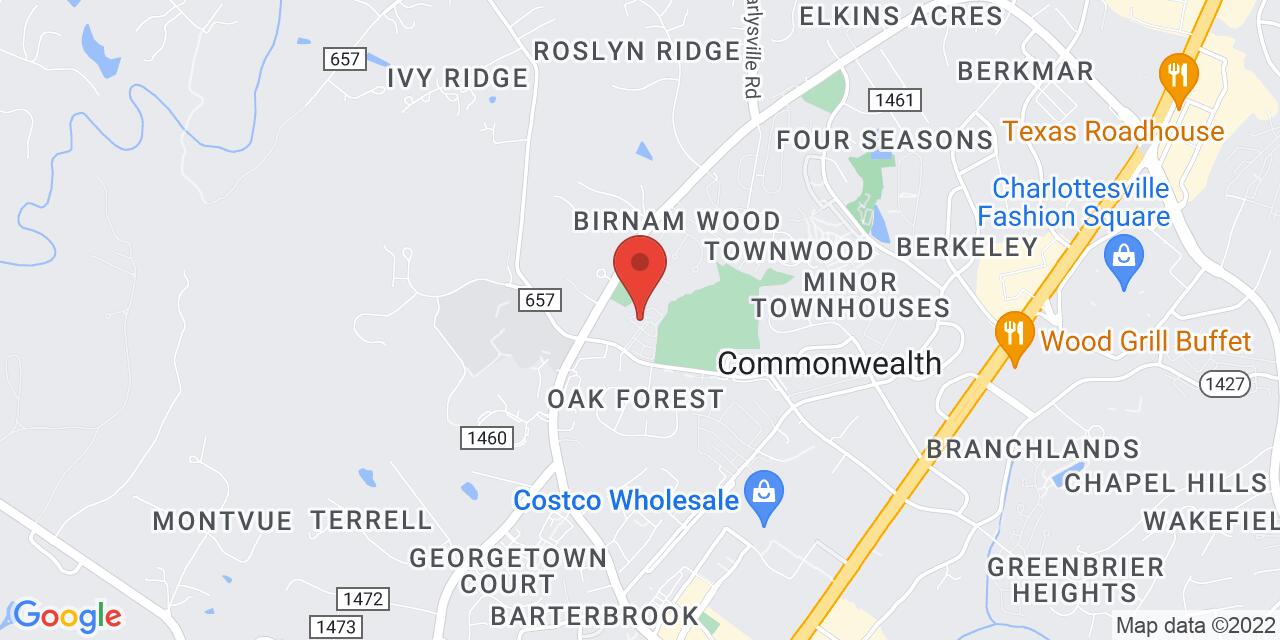
Call (434) 978-3100 today or click here to schedule a free consultation.